What Are Piles And What Causes Them?
Piles are swellings that can occur in the anus and lower rectum (back passage).
There is a network of small veins (blood vessels) within the inside lining of the anus and lower rectum. These veins sometimes become wider and engorged with more blood than usual. These engorged veins and the overlying tissue may then form into one or more small swellings called piles
The exact reason why these changes occur and lead to piles forming is not clear. Some piles seem to develop for no apparent reason. However, it is thought that the pressure in and around the anus can be a major factor in many cases. If the pressure in and around the anus is increased, then it is thought that this can lead to piles developing. Certain situations increase the chance of haemorrhoids developing.
Constipation, passing large stools (faeces), and straining at the toilet. These increase the pressure in and around the veins in the anus and seem to be a common reason for piles to develop
Piles are common during pregnancy. This is probably due to pressure effects of the baby lying above the rectum and anus, and the affect that the change in hormones during pregnancy can have on the veins.
The tissues in the lining of the anus may become less supportive as we get older.
Some people may inherit a weakness of the wall of the veins in the anal region.

What Are The Symptoms Of Haemorrhoids / Piles ?
Internal haemorrhoids
These form in the back passage about 2-4 cm above the rim (opening) of the anus. Their severity and size are classified into grades 1 to 4.
are small swellings on the inside lining of the back passage. They cannot be seen or felt from outside the anus. Grade 1 piles are common. In some people they enlarge further to grade 2 or more.
are larger. They may be partly pushed out (prolapse) from the anus when you go to the toilet, but quickly ‘spring back’ inside again.
hang out (prolapse) from the anus. You may feel one or more as small, soft lumps that hang from the anus. However, you can push them back inside the anus with a finger.
permanently hang down from within the anus, and you cannot push them back inside. They sometimes become quite large.
Symptoms can vary. Small haemorrhoids are usually painless. The most common symptom is bleeding after going to the toilet. Larger haemorrhoids may cause a mucus discharge, some pain, irritation, and itch. The discharge may irritate the skin around the anus. You may have a sense of fullness in the anus, or a feeling of not fully emptying your rectum when you go to the toilet.
A possible complication of Piles that hang down (grade 3-4) is a blood clot (thrombosis) which can form within the haemorrhoid. This is uncommon, but causes intense pain if it occurs.
External haemorrhoid (sometimes called a perianal haematoma)
This is less common than internal haemorrhoids. An external haemorrhoid is a small lump that develops on the outside edge of the anus. Many do not cause symptoms. However, if a blood clot forms in the haemorrhoid (‘thrombosed external haemorrhoid’) it can suddenly become very painful and need urgent treatment. The pain due to a thrombosed external haemorrhoid usually peaks after 48-72 hours, and then gradually goes away over 7-10 days. A thrombosed external haemorrhoid may bleed a little for a few days. It then gradually shrinks to become a small skin-tag.
Some people develop internal and external haemorrhoids at the same time.
What Is The Treatment For Haemorrhoids / Piles ?
- Eat plenty of fibre such as fruit, vegetables, cereals, wholemeal bread, etc.
- Have lots to drink. Adults should aim to drink at least two litres (10-12 cups) per day. You will pass much of the fluid as urine, but some is passed out in the gut and softens faeces. Most sorts of drink will do, but alcoholic drinks can be dehydrating and may not be so good.
- Fibre supplements. If a high fibre diet is not helping, you can take bran, or other fibre supplements (‘bulking agents’) such as ispaghula, methylcellulose, or sterculia. You can buy these at pharmacies or get them on prescription. Methylcellulose also helps to soften faeces directly which makes them easier to pass.
- Avoid painkillers that contain codeine such as co-codamol, as they are a common cause of constipation.
- Toileting. Go to the toilet as soon as possible after feeling the need. Some people suppress this feeling and plan to go to the toilet later. This may result in bigger and harder faeces forming which are then more difficult to pass. Do not strain on the toilet. Piles may cause a feeling of ‘fullness’ in the rectum and it is tempting to strain at the end to try and empty the rectum further. Resist this. Do not spend too long on the toilet which may encourage you to strain. (For example, do not read whilst on the toilet.)
The above measures will often ease symptoms such as bleeding and discomfort. It may be all that you need to treat small and non-prolapsing haemorrhoids (grade 1).
Various preparations and brands are commonly used. They do not ‘cure’ Piles . However, they may ease symptoms such as discomfort and itch.
- A bland soothing cream, ointment, or suppository may ease discomfort. Several brands are available without a prescription. Ask a pharmacist to advise. Follow the instructions on the packet on how to use.
- One that contains an anaesthetic may ease pain better. You should only use one of these for short periods at a time (5-7 days). If you use it for longer, the anaesthetic may irritate or sensitise the skin around the anus. A pharmacist can advise.
- One that contains a steroid may be advised by a doctor if there is a lot of inflammation around the haemorrhoids. Steroids reduce inflammation and may help to reduce any swelling around a haemorrhoid. This may help to ease itch and pain. You should not normally use a steroid cream or ointment for longer than one week at a time.
- Very painful prolapsed haemorrhoids are uncommon. The pain may be eased by an ice pack pressed on for 15-30 minutes. Strong painkillers may be needed.
- Haemorrhoids of pregnancy usually settle after the birth of the child. Treatment is similar to the above.
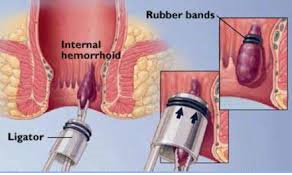
Banding Treatment
Banding is a common treatment for grade 2 and 3 Piles. It may also be done to treat grade 1 Piles which have not settled with the measures described above (such as an increase in fibre, etc).
This procedure is usually done by a surgeon in an outpatient clinic. A haemorrhoid is grasped by the surgeon with forceps or a suction device. A rubber band is then placed at the base of the haemorrhoid. This cuts off the blood supply to the haemorrhoid which then ‘dies’ and drops off after a few days. The tissue at the base of the haemorrhoid heals with some scar tissue.
Banding of internal haemorrhoids is usually painless as the base of the haemorrhoid originates above the anal opening – in the very last part of the gut where the gut lining is not sensitive to pain. Up to three haemorrhoids may be treated at one time using this method.
In about 8 in 10 cases, the haemorrhoids are ‘cured’ by this technique. In about 2 in 10 cases, the haemorrhoids recur at some stage. (However, you can have a further banding treatment if this occurs.) Banding does not work in a small number of cases. Haemorrhoids are less likely to recur after banding if you do not become constipated and do not strain on the toilet (as described above).
A small number of people have complications following banding such as bleeding, urinary problems, or infection or ulcers forming at the site of a treated hemorrhoid.
Injection Sclerotherapy
Phenol in oil is injected into the tissues at the base of the haemorrhoids. This causes a fibrotic (scarring) reaction which obliterates the blood vessels going to the haemorrhoids. The haemorrhoids then ‘die’ and drop off similar to after banding. However, this procedure is less widely used than banding because the success rate is not as good.
Various methods that use heat to ‘destroy’ the haemorrhoids
There are various ways this can be done and include: infrared coagulation; photocoagulation; diathermy; electrotherapy. However, these procedures are less widely used than banding because their success rate is not as good.
Haemorrhoidectomy
Haemorrhoidectomy (the traditional operation)
An operation to cut away the haemorrhoid(s) is an option to treat grade 4 haemorrhoids, and for grade 2 and 3 haemorrhoids not successfully treated by banding or other methods. The operation is done under general anaesthetic and is usually successful. However, it can be quite painful in the days following the operation.
Stapled Haemorrhoidectomy
Although the name of this procedure implies that the haemorrhoids / piles are removed (cut out), this is not so. What happens in this procedure is a circular stapling ‘gun’ is used to cut out a circular section of the lining of the anal canal above the haemorrhoids. This has an effect of pulling the haemorrhoids back up the anal canal. It also has an effect of reducing the blood supply to the haemorrhoids which shrink as a consequence. Because the ‘cutting’ is actually above the haemorrhoids, it is usually a less painful procedure than the traditional operation to remove the haemorrhoids.
THD – The Procedure
A Minimally Invasive Procedure
THD uses a doppler to locate the terminating branches of the hemorrhoidal arteries. Once the artery is located the surgeon uses an absorbable suture to ligate or “tie-off” the arterial blood flow. The venous “out flow” remains to “shrink” the cushion. This is done without excision of tissue. If necessary the surgeon will perform a hemorrhoidopexy to repair the prolapse. Again, this is done with suture and no excision of tissue. This repair restores and “lifts” the tissue back to its anatomical position.
The entire procedure is performed above the dentate line so that there is minimal discomfort. The procedure takes about 20 minutes and is offered as an out-patient surgery
Laser Procedure for Haemorrhoids / Piles
This is mainly for grade 2 and early grade 3 haemorrhoids. Here a device is used to supply a diode laser current to the pile mass to help it shrink. It still requires a short anaesthetic but the post operative pain is less.