Ulcerative Colitis
Ulcerative Colitis (UC) is a disease where inflammation develops in the large intestine (the colon and rectum). The most common symptom when the disease flares up is diarrhoea mixed with blood. When a flare-up occurs, treatment can usually ease symptoms. The disease can often be prevented from flaring up by taking medication, usually mesalazine, each day. Surgery to remove the colon is needed in some cases. People with UC have an increased risk of developing colon cancer. This risk is reduced by taking mesalazine each day. After 8-10 years, an inspection inside the colon every 1-3 years using a colonoscope (flexible telescope) is usually advised to screen for pre-cancer changes.
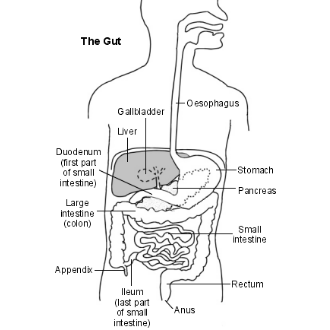
Understanding The GUT
The Gut (Gastrointestinal Tract) is the long tube that starts at the mouth and ends at the anus.
Food passes down the oesophagus (gullet), into the stomach, then into the small intestine.
The small intestine has three sections – the duodenum, jejunum and ileum. The small intestine is where food is digested and absorbed into the bloodstream. The structure of the gut then changes to become the large intestine (colon and rectum, sometimes called the large bowel).
The colon absorbs water, and contains food that has not been digested, such as fibre. This is passed into the last part of the large intestine where it is stored as faeces.
Faeces (motions or stools) are then passed out of the anus into the toilet.
What Is Ulcerative Colitis (UC)?
- Colitis means ‘inflammation of the colon’.
- Ulcerative means that ulcers tend to develop, often in places where there is inflammation. An ulcer is where the lining of the gut is damaged and the underlying tissue is exposed. If you could see inside your gut, an ulcer looks like a small, red crater on the inside lining of the gut. Ulcers that occur in UC develop in the large intestine and have a tendency to bleed.
The inflammation and ulcers in the large intestine cause the common symptoms of diarrhoea, and passing blood and mucus.
Who Gets Ulcerative Colitis ?
About 1 in 1000 people in the UK develop UC. It can develop at any age but most commonly first develops between the ages of 15 and 40. About 1 in 7 cases first develop in people over the age of 60.
The cause is not known. UC can affect anyone. About 1 in 5 people with UC have a close relative who also has UC. So, there is probably some genetic factor. The common theory is that some factors may ‘trigger’ the immune system to cause inflammation in the large intestine in people who are genetically prone to develop the disease.
The most likely ‘trigger’ for UC to develop is a bacterium or virus (germ). However, it is not clear which bacterium or virus is the culprit. But other triggers that may cause a flare-up of UC to include anti-inflammatory drugs and withdrawal from nicotine in people who give up smoking. In people who are known to have UC, a common trigger for a flare-up of symptoms is about gastroenteritis (infection of the gut) caused by various bacteria.
- Diarrhoea. This varies from mild to severe. The diarrhoea may be mixed with mucus or pus. An urgency to get to the toilet is common. A feeling of wanting to go to the toilet but with nothing to pass is also common (tenesmus). Water is not absorbed so well in the inflamed colon, which makes the diarrhoea watery
- Blood mixed with diarrhoea is common (‘bloody diarrhoea’).
- Crampy pains in the abdomen.
- Pain when passing stools.
- Proctitis (inflammation of the rectum). Symptoms may be different if a flare-up only affects the rectum, and not the colon. You may have fresh bleeding from the rectum, and you may form normal stools rather than have diarrhoea. You may even become constipated further ‘upstream’ in the unaffected higher part of the colon, but with a frequent feeling of wanting to go to the toilet.
- Feeling generally unwell is typical if the flare-up affects a large amount of the large intestine, or lasts a long time. Fever, tiredness, feeling sick, weight loss, and anaemia may develop
How Does Ulcerative Colitis Progress?
UC is a chronic, relapsing condition. Chronic means that it is persistent and ongoing. Relapsing means that there are times when symptoms flare-up (relapse), and times when there are few or no symptoms (remission). The severity of symptoms, and how frequently they occur, varies from person to person. The first episode (flare-up) of symptoms is often the worst.
UC starts in the rectum in most cases. This causes a proctitis, which means ‘inflammation of the rectum’. In some cases it only affects the rectum, and the colon is not affected. In others, the disease spreads up to affect some, or all, of the colon. Between flare-ups the inflamed areas of colon and rectum heal, and symptoms go away. The severity of a flare-up can be classed as mild, moderate or severe
| Mild | You have fewer than four stools (motions) daily, with or without blood. You do not feel generally unwell (‘no systemic disturbance’). |
| Moderate | You have four to six stools a day and feel mildly unwell in yourself (‘minimal systemic disturbance’). |
| Severe | You have more than six stools a day containing blood. You also feel generally unwell with more marked ‘systemic disturbance’ with things such as fever, a fast pulse, anaemia, etc. |
About half of people with UC have mild and infrequent symptoms. The other half have more frequent flare-ups with moderate or severe symptoms. During a flare-up, some people develop symptoms gradually – over weeks. In others, the symptoms develop quite quickly – over a few days.
Are There Any Complications With Ulcerative Colitis?
A very severe flare-up
This is uncommon, but if it occurs it can cause serious illness. In this situation, the whole of the large intestine becomes ulcerated, inflamed, and dilated (megacolon). A part of the colon may perforate (puncture), or severe bleeding may occur. Urgent surgery may be needed if a flare-up becomes very severe and is not responding to medication (see later).
Related conditions
Other problems in other parts of the body occur in about 1 in 10 cases. It is not clear why these occur. The immune system may trigger inflammation in other parts of the body when there is inflammation in the gut. These ‘ outsides of the gut’ problems include
- Those that may flare up when gut symptoms flare up. That is, they are related to the activity of the colitis and go when the gut symptoms settle. These include
- Erythema nodosum (an unusual rash on the legs)
- Aphthous ulcers (mouth ulcers).
- Episcleritis (a type of eye inflammation).
- Acute arthropathy (painful joints).
- Those that are usually related to the activity of the colitis and usually go, but not always, when the gut symptoms settle. These include
- Pyoderma gangrenosum (an unusual skin condition).
- Anterior uveitis (a type of eye inflammation).
- Those that are not related to the activity of the colitis. So, they may persist even when the gut symptoms settle. These include
- Sacroiliitis (inflammation of the joints between the sacrum and the lower spine).
- Ankylosing spondylitis (a type of arthritis that affects the spine).
- Primary sclerosing cholangitis (which causes inflammation of the bile ducts of the liver).
Dignosis
The usual test is for a doctor to look inside the large intestine by passing a special telescope up through the anus into the rectum and colon. These are a short sigmoidoscope or a longer flexible colonoscope. See separate leaflets called ‘Colonoscopy’ and ‘Sigmoidoscopy’ for more detail. The appearance of the inside lining of the rectum and colon may suggest UC. Small samples (biopsies) are taken from the lining of the rectum and colon and looked at under the microscope. The typical pattern of the cells seen with the microscope may confirm the diagnosis. Also, various blood tests are usually done to check for anaemia and to assess your general wellbeing.
Special X-ray tests such as a barium enema are not often done thesedays as the above tests are usual to confirm the diagnosis, and assess the disease severity.
A stool sample (sample of faeces) is commonly done during each flare-up and sent to the ‘lab’ to test for bacteria and other infecting germs. Although no germ has been proven to initially cause UC, infection with various known germs can trigger a flare-up of symptoms. If a germ is found, then treatment of this may be needed in addition to any other treatment for a flare-up (described below).
What Are The Treatment Options For A Flare-Up Of Ulcerative Colitis?
These include mesalazine, olsalazine, balsalazide and sulfasalazine. The active ingredient of each of these drugs is 5-aminosalicylic acid, but each drug is different in how the active ingredient is released or activated in the intestine. Mesalazine is the most commonly used. Each of these drugs comes in different brand names and different preparations such as oral tablets, sachets or suspension, liquid or foam enemas, or suppositories. The type of preparation (for example, tablets or enemas) may depend on the main site of the inflammation in the intestine.
Aminosalicylate drugs often work well for mild flare-ups. The exact way these drugs work is not clear but they are thought to counter the way inflammation develops in UC. However, they do not work in all cases. Some people need to switch to steroid medication if an aminosalicylate drug is not working, or if the flare-up is moderate or severe.
Side-effects with the more modern aminosalicylate drugs (mesalazine, olsalazine, and balsalazide) are uncommon. The older drug, sulfasalazine, had a higher rate of side-effects so is not commonly used these days.
Steroids work by reducing inflammation. If you develop a moderate or severe flare-up of UC a course of steroid tablets (corticosteroids) such as prednisolone will usually ease symptoms. The initial high dose is gradually reduced and then stopped once symptoms ease. A steroid enema or suppository is also an option for a mild flare-up of proctitis. Steroid injections directly into a vein may be required for a severe flare-up.
A course of steroids for a few weeks is usually safe. Steroids are not usually continued once a flare-up has settled. This is because side-effects may develop if steroids are taken for a long time (several months or more). The aim is to treat any flare-ups but to keep the total amount of steroid treatment over the years as low as possible.
Powerful drugs that suppress the immune system (immunosuppressants) may be used if symptoms persist despite the above treatments. For example, azathioprine, cyclosporin, or infliximab are sometimes needed to control a flare-up of UC.
Although most people with UC have diarrhea during a flare-up, as mentioned ‘high’ constipation may develop if you just have proctitis (inflammation of the rectum only). In this situation, laxatives to clear any constipation may help to ease a flare-up of proctitis.
Note: antidiarrhoeal medication such as loperamide should NOT be used during a flare-up of UC. This is because they do not reduce diarrhea that occurs with UC and increase the risk of developing megacolon (a serious complication of UC – see below).
What Are The Treatment Options To Prevent Flare-Ups Of Symptoms?
Once an initial flare-up of symptoms has cleared, you will usually be advised to take a drug each day to prevent further flare-ups. If you have UC and do not take a regular preventive drug, you have about a 7 in 10 chance of having at least one flare-up each year. This is reduced to about a 3 in 10 chance if you take a preventative drug each day.
An aminosalicylate drug, usually mesalazine (described above), is commonly used to prevent flare-ups. A lower ‘maintenance dose’ than the dose used to treat a flare-up is usual. You can take this indefinitely to keep symptoms away. Most people have little trouble taking one of these drugs as side effects are uncommon. However, some people develop side-effects such as abdominal pains, feeling sick, headaches, or rashes.
If a flare-up develops whilst you are taking an aminosalicylate drug then the symptoms will usually quickly ease if the dose is increased, or if you switch to a short course of steroids. Another drug may be advised if an aminosalicylate drug does not work, or causes difficult side-effects. For example, azathioprine or 6-mercaptopurine are sometimes used.
Probiotics are nutritional supplements that contain ‘good’ bacteria. That is, bacteria that normally live in the gut and do no harm. Taking probiotics may increase the ‘good’ bacteria in the gut which may help to ward off ‘bad’ bacteria that may trigger a flare-up of symptoms. There is little scientific proof that probiotics work to prevent flare-ups. However, a probiotic strain (Escherichia coli Nissle 1917) and the probiotic preparation VSL3 have shown promise. Further research is needed to clarify the role of probiotics.
Unfortunately, not everyone with UC has their symptoms well controlled with medication. About a quarter of people with UC need surgery at some stage. The common operation is to remove the large intestine. There are different techniques used for this. It is helpful to discuss the pros and cons of the different operations with a surgeon. Removing the large intestine will usually cure symptoms of UC permanently.
Surgery is considered in the following situations.
- During a life-threatening flare-up. Removing the large intestine may be the only option if it swells greatly (‘megacolon’), perforates (punctures), or bleeds uncontrollably.
- If UC is poorly controlled by medication. Some people remain in poor health with frequent flare-ups which do not settle properly. To remove the large intestine is a serious step, but for some people the operation is a relief after a long period of ill health.
- If cancer or ‘pre-cancer’ of the large intestine develops.
Types Of Surgery
Surgical treatment can be broadly divided into surgery which leaves you with a permanent bag ie total colectomy with ileostomy or total colectomy with an ileoanal pouch where you make a new rectum for the patient out of small bowel
Total Colectomy And Ileostomy
This is essentially a curative operation for the disease as you remove all large bowel where the disease is present and there is no recurrence. This is a major operation which used to require a large cut in the belly and a permanent bag
At the laparoscopic clinic, this can be done by keyhole, and you are left with only 4-5 small cuts in the belly. The recovery is much faster and you can eat and drink on the same day compared to fasting after a big operation
Total Colectomy And Ileoanal Pouch
This is an operation that can be offered to younger patients who do not want a bag for life. This might have to be done as a two or three-stage operation
In the first operation, you remove most of the bowel away leaving a small amount behind. Then at the second operation, you remove the lower end of the bowel and join the small bowel to the anal canal by forming a pouch which acts as the new rectum
After the operation, the patient may move his bowels normally 6-7 times a day. He or she will need surveillance of the lower end of the bowel once a year
This operation is technically more difficult but can be done at this clinic by a laparoscopic-assisted technique which again offers patient faster recovery and less pain
General Treatment Measures
- A special diet is not usually needed. A normal, healthy, well balanced diet is usually advised. If you have UC just in the rectum (proctitis), a high fibre diet may help to avoid constipation.
- You may be advised to take iron tablets if you develop anaemia.
- You may need painkillers when symptoms flare-up
Ulcerative Colitis And Cancer Of The Colon
The chance of developing cancer of the large intestine (colon) is higher than average in people who have had Ulcerative colitis for several years or more. It is more of a risk if you have frequent flare-ups affecting the whole of the large intestine. For example, about 1 in 10 people who have Ulcerative colitis for 20 years which affects much of their large intestine will develop cancer.
Because of this risk, people with Ulcerative colitis are usually advised to have their large intestine routinely checked after having had Ulcerative Colitis for about 8-10 years. This involves a look into the large intestine by a flexible telescope (colonoscopy) every now and then. Your specialist will advise exactly how often you should have this test. Commonly, a colonoscopy is done every three years in people who have had Ulcerative Colitis for 10-20 years, every two years in people who have had Ulcerative colitis for 20-30 years, and every year in people who have had Ulcerative colitis for 30 or more years. But there are exceptions to this ‘rule of thumb’ and your specialist will advise.
In most cases, any changes are noticed from biopsies (small samples) taken during colonoscopy long before any cancer develops. (This is a similar principle to cervical screening in women.) If changes are found, surgery to remove the large intestine is advised to prevent cancer developing.
Recent studies indicate that the risk of cancer is reduced in people who take regular long-term aminosalicylate medication (described above). In one study, patients with ulcerative colitis who regularly took mesalazine had a 75% reduced risk of developing colon cancer.
What Is The Prognosis (Outlook)?
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis compared to the general population. After this there is little difference in life expectancy from the general population. However, a severe flare-up of UC is still a potentially life threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with UC have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with UC eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with UC are fully capable of work. So, this means that in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near normal life. However, UC causes significant employment problems for a minority.
Treatment for UC is an evolving field. Various new drugs are under investigation and may change the treatment options over the next ten years or so, and improve the prognosis.